A primer’s introduction to Leonhard’s classification of endogenous psychoses for ICD/DSM formatted minds
While providing some success in applied medicine, the DSM failed in basic science. This motivated the shift from the “naturalistic” paradigm of traditional scientific medicine, to the “normativistic” paradigm for diseases. However, the failure could rather be due to the endorsement of inappropriate phenotypes. Indeed, in scientific medicine, good phenotypes to start with should be more than reliable, they ought to have some natural foundations.
The Wernicke-Kleist-Leonhard school has tried to identify such natural phenotypes especially in the schizophrenia and affective spectra. Those have been elaborated on diachronic observations, using three key principles to optimize the description process. First, the elementary symptom principle which integrates symptoms in symptom-complexes. In second instance, the longitudinal principle allows to definite phenotypes, i.e. symptom-complex with typical course and outcome. One patient is assigned to one phenotype only which accounts for his full clinical picture. Thirdly, the familial aggregation principle which assumes the phenotype to be the same in multiplex families. This results in 35 major phenotypes of good reliability, but also good predictive validity and good differential validity concerning age of onset, heritability, fetal event and treatment response. These phenotypes should be inspiring for the next generation of scientists in psychosis research.
Authors: Jack Foucher, Fabrice Berna, Markus Hanke, Alexandre Obrecht & Bruno Pfuhlmann
Introduction
The field of endogenous psychoses is the one for which the hypothesis of a “cerebral disease” is the most likely in psychiatry. Unfortunately, according to David Kupfer, task-force leader of the DSM-5, the “slavish adoption” of the DSM during the past 40 years has dug the grave of the traditional medical science approach. The defined entities turned out to be disappointing phenotypes and two postulates of the DSM made it unsuitable for research. First, criteria could not be changed impeding any attempt to optimize the phenotypical descriptions. Second, the a-theoretical stance excluded even crude etiological or pathophysiological hypothesis resulting from the blending of endogenous and neurotic forms. Yet the traditional paradigm of scientific medicine, which could be called the naturalistic paradigm of pathological dysfunction, states that a disease is a natural entity which is defined by an explanatory causal model for clinical manifestations. The model is given at the biological level, i.e. at a different level than the phenomenological one, as a dysfunction of a physiological process or as its cause, in other words, its pathophysiology or its etiology. This model can therefore be validated by discovering the dysfunctional process accounting for the whole characteristic features of the phenotype. Such validation generally starts with the correlation method, that attempts to find a robust and specific association of the putative phenotype with biological or physiological biomarkers for the dysfunction, e.g. pathology, biochemistry, immunology, electrophysiology or genetic. The model is even more convincingly validated by the experimental method, either by reproducing clinical manifestations when inducing the causal dysfunction in animals or by removing them when correcting the causal dysfunction. In physician’s hands, biomarkers become screening tests while corrective experiments become therapies.
The recurrent failures to validate ICD or DSM entities gave birth to a great doubt about the traditional paradigm of scientific medicine in psychiatry. The leading proposal is even to turn towards dimensional approaches, without considering the paradigmatic change that comes along, i.e. the adoption of the normativistic paradigm of pathological deviance. Here, pathology is rephrased as abnormality, defined as the deviation of a trait or a dimension from the norm. It makes the implicit assumption of multiple causes of very small effects. Although useful for the study of complex traits in normal populations as in psychology or population genetics, it is inappropriate to discover morbid entities coming from a single and specific cause. It is thus not surprising that this paradigm did not allow to re-discover already known diseases, e.g. Parkinson’s disease vs supranuclear palsy.
Yet the failure of the traditional paradigm of scientific medicine might only be due to the use of inappropriate phenotypes to begin with. Here, we define a phenotype as a set of observable characteristics that are so “typically” shared by a group of patients that they naturally cluster together. This includes the clinical presentation, i.e. the set of symptoms and clinical signs observed when the patients are examined, and its specific course, i.e. how symptoms appeared, which ones persist, which ones disappeared or the complete change from one clinical picture to another that might even be its opposite etc. Finally, typical contextual elements might also enrich the description of a phenotype: age of onset, familial aggregation, risk factors, treatment response, etc.
What properties should have a phenotype to be a good candidate for the validation process to start with? Since the ICD-8/9 and the DSM-III were purely technical the only property required was reliability, i.e. having a good inter-rater reproducibility. But reliability alone is not enough. Good phenotypes to start with should have some natural clustering foundations. These can only be ensured by the optimization of their description based on clinical observations and can be further ascertained by fulfilling other properties. A first property of a chronic phenotype is its stability. Even if the clinical manifestations change from time to time in the same patient, the simplest and most likely hypothesis assumes that he is presenting with only one disease and not with two or three different ones. A second property of a natural phenotype is its face validity or plausibility, i.e. how far new clinical observations match the “typical” definition and how far this “typical” definition accounts for all the patient’s manifestations. A third property that can be derived from stability and face validity is the ability to anticipate the course of the illness according to its phenotypic description, that is predictive validity. Test-retest reproducibility can be used as a measure of predictive validity. Finally, the fourth property is the specific association of the phenotype with an “external validator”, which is a clinical or contextual feature, that is not part of the original description, e.g. heritability, gender difference, treatment response etc. This differential validity is assessed by the head to head comparison of the validator’s association with at least two phenotypes. The basic heuristic of classical medicine to define natural phenotypes has always been the optimization of several of the above-mentioned properties. This supposes an empirical construction by means of a constant back and forth between observation and description. Yet, international classifications were not built empirically but through consensus, a process that rather promotes minimal common knowledge, which for endogenous psychoses was the Kraepelinian dichotomy. For historical reasons, reliability was the only property that had been optimized in their development at the expense of validity. But concluding from the failure of Spitzer’s DSM-project that there are no natural phenotypes in the field of endogenous psychoses comes with the risk to throw the baby out with the bathwater. Our purpose here is to offer a reminder to the psychosis research community of what the Wernicke-Kleist-Leonard (WKL) school phenotypes were all about, as stated in the last version of Leonhard’s classification. The WKL school introduced the distinction between bipolar and unipolar disorders. But the version which was later endorsed by the ICD/DSM, is a dramatic oversimplification of the original one. After an introduction to the classification, stressing its differential and predictive validity, we will underline the principles that have guided its empirical construction. Finally, we will report its reliability and stability.
Introduction to the WKL classification
Conceptual frame
The WKL classification concerns endogenous psychoses. “Psychosis” does not have the same meaning here than in the DSM or the ICD, i.e. it is not restricted to a disturbance in the relation with reality such as hallucinations or delusion. In the WKL perspective, the term psychosis stands for a wide range of emotional, cognitive and behavioral disturbances that can be accounted for by some qualitative disturbances of some cerebral processes either due to a structural (organic) or functional (endogenous or exogenous) pathologies. It is opposed to the old concept of “neuroses” that are disturbances which result from “normal” albeit maladaptive brain processing due to the interaction of a given personality in a given context. Most, but not all the WKL’s phenotypes are within the scope of ICD/DSM’s affective and psychotic disorders, e.g. some can also fit within the autistic spectrum or personality disorders. The term endogenous should be put in the perspective of Kraepelin’s, Birnbaum or Jaspers’ tripartite system in which psychiatric symptoms could be organic (exogenous, i.e. secondary to a medical condition including substance related), reactive (neurotic) or functional (endogenous). The latter means that no medical condition or psychodynamic context can better account for the clinical manifestations. Endogeneity suggests a cryptogenic nature, i.e. a brain disorder which still has to be discovered. While the ICD and the DSM still distinguish exogenous disorders, the endogenous - neurotic distinction has completely disappeared due to the a-theoretic principle. On the “psychotic” side, psychotic post-traumatic stress disorder, psychotic body dysmorphic disorder or stress related brief psychotic reactions as observed in borderline personality disorder, do not correspond to endogenous psychoses. But the largest difference between WKL and ICD/DSM classifications is on the “affective” side, as reactive and neurotic depressions, e.g. grief of secondary to an earlier abuse, are not included in WKL endogenous psychoses.
Presentation of the classification
For an ICD/DSM trained mind, the understanding of the classification requires the acceptance to step back and to get a different point of view. This new perspective should not consider so much what the phenotypes have in common, but rather in what aspect they differ one from another. Indeed, there are many phenotypes in which psychosis, in the ICD/DSM sense, is not central but essentially a non-specific manifestation, as psychotic symptoms secondary to a medical condition. Conversely, when psychotic symptoms, in the ICD/DSM sense, are the core of the phenotype, they have specific features which excludes the other ones.
The WKL classification describes 35 “major” phenotypes grouped in 5 families. These a strikingly different from the ICD / DSM’s categories up to the point that even the WKL’s families are poorly concordant with the international classifications, i.e. concordance λ = 0.4 and 0.56 with the ICD-10 and the DSM-IV respectively while the latter have a concordance λ = 0.86. There is such a bulk of symptoms and clinical signs specific for each WKL’s diagnosis that any attempt to explore them systematically on a checklist basis is challenging. Previous attempts failed probably because symptoms have no meaning by themselves in the WKL perspective, but only as part of a symptom-complex. Most of the time the phenotypical diagnosis can be reasonably pinpointed at the end of the first episode, but diagnosis accuracy is further ascertained when long term follow-up is available. The diachronic reconstruction should allow to itemize the course (i.e. relapsing-remitting, progressive-relapsing or primary progressive), and to specify acute and residual clinical manifestations (e.g. monomorphic vs polymorphic).
The following presentation of the WKL classification has been necessarily simplified. It is summarized in table 1 according to a practical division based on the most affected neuropsychological domain: affect, thought and psychomotor domains.
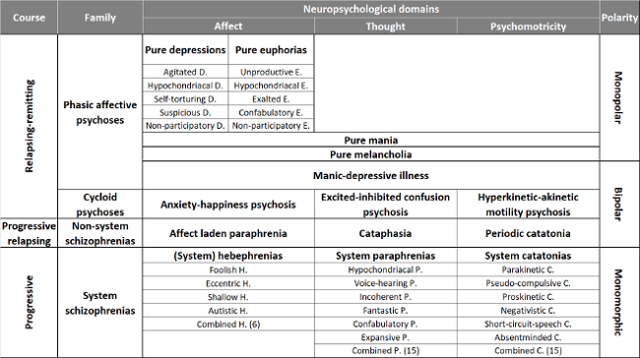
Table 1. Overview of the WKL phenotypes. Only the 35 major forms are displayed, the 36 minor forms are two by two combinations of system schizophrenias.
Monopolar phenotypes with purely relapsing-remitting course
Pure melancholia and pure mania
Pure melancholia and pure mania are monopolar mood disorders. The term monopolar is used here rather than “unipolar” to remind the differences between the original WKL’s concept and the ICD/DSM’s one. First, monopolarity concerns not only the melancholic but also the manic pole although this are rare cases. Subsequently, it implies symptomatic stability or monomorphy, and finally, the absence of mixed or incomplete states (see manic-depressive psychosis). Conversely, the ICD/DSM’s unipolar disorder gives no clinical clue for the differential diagnosis with bipolar forms. Unipolarity only concerns the depressive pole, despite the independent confirmation of pure mania in the Zurich cohort. It merely points that up to the day of the examination, the patient should have experienced depressive episodes only.
Pure melancholia overly prevails as it concerns up to 10% of all endogenous psychoses, whereas pure mania is largely below one percent. The course is purely relapsing-remitting although episodes can last for years, especially for pure mania. Symptoms typically respond to usual therapeutics. Pure melancholia and pure mania have very little inheritance with about 3% of affected first degree relatives contrary to manic-depressive psychosis.
Pure depressions and pure euphorias
These are also monopolar phenotypes, i.e. the same clinical picture is observed along the same episode, remains the same on recurrences and presents no clinical features of the other pole. The 5 pure depressions and the rare 5 pure euphorias are characterized by specific disturbances of distinct systems within the affective domain without involvement of drive and psychomotor activity. They do have more frequently “psychotic” content, in the sense of ICD/DSM, but of a very specific kind. In fact, specific “psychotic” symptoms must even be observed in some phenotypes: a special kind of delusional guilt in self-tortured depression, a specific type of persecutory ideas in suspicious depression and specific unpleasant bodily sensations in hypochondriacal depression.
There is no problem for diagnosing agitated depression as an ICD/DSM affective disorder. Conversely, non-participatory depressions might rather be diagnosed as a chronic depersonalization disorder. The three others may be diagnosed as schizo-affective disorders. These phenotypes are observed in about 4% of inpatients with endogenous psychoses. Episodes can last up to several years, frequently with very progressive beginnings and endings. Symptoms are less responsive to therapeutics than pure melancholia. At last, there is a very low family burden associated with them, compared to manic-depressive psychoses, 3% vs. 22-36%.
Bipolar phenotypes with purely relapsing-remitting course
The WKL concept of manic-depressive psychosis, or MDP, should be distinguished from the Kraepelinian manic depressive madness (“manisch-depressives Irresein”) and the ICD / DSM concept of bipolar disorders. The WKL school not only separates bipolar phenotypes from monopolar phenotypes that were merged according to the Kraepelinian concept, but proposes seven bipolar and twelve monopolar phenotypes. MDP is only one of these bipolar forms, beside three cycloid psychoses and three non-system schizophrenias. Among them, MDP is the only purely affective and the most frequent phenotype, accounting for about 19% of patients with endogenous psychosis. Although MDP might look as the archetype of bipolar disorders, there are many differences between the WKL and the ICD/DSM concepts. Firstly, clinical features enable to distinguish pure mania from MDP contrary to ICD/DSM’s bipolar disorder. Secondly, many patients can only have depressive recurrences and still be diagnosed with MDP, again thanks to the specific features of MDP’s depressive manifestations which are rediscovered in the emerging concept of “bipolar depression”. Ultimately, MDP has been separated from cycloid psychoses and non-system schizophrenias, while some cases of these can be diagnosed as ICD/DSM’s bipolar disorder.
The span of MDP’s clinical presentations is very large, and it can mimic any monopolar phenotype. But one specific feature of this phenotype is its polymorphic presentation, i.e. clinical manifestations that are changing within and between episodes. The trigger for these changes can be endogenous, but these patients are also sensitive to the context which can trigger mood, thought and/or psychomotor reactivity. For instance, patients can be talkative and lively during the interview, showing no outer manifestation of depression, while apathy and mental suffering come back as soon as they walk out of the office. The differential diagnosis must be done with neurotic forms which may also exhibit some mood reactivity (although of lower magnitude), whereas MDP episodes may well be triggered by inner conflicts or emotional life events.
Another feature of MDP manifestations is their mixed or incomplete character. Mixed means that there is an inhomogeneous combination between the three neuropsychological domains: affect, thoughts and psychomotricity, e.g. sadness (inhibited affect) mixed with racing thoughts (excited thinking process) and agitation (excited psychomotricity). The WKL concept of incompleteness is an extension of the former, meaning that neuropsychological domains can be very unequally affected and some can even be spared, e.g. sadness (inhibited affect) with inhibited psychomotricity but normal speed of thought (normal thinking process).
On average, MDP’s episodes are of shorter duration than the ones of monopolar affective phenotypes, i.e. about half. However, this does not prevent some episodes to last a very long time, especially when the clinical picture is an agitated depression or a non-participatory depression. An acute beginning and a sudden ending are very indicative for an MDP episode. The relapses are also more frequent with shorter inter-episode intervals than monopolar disorder which further tends to decrease with aging.
The hereditary burden is significantly higher than for monopolar phenotypes, with 22 to 36% of affected first degree relatives. This percentage is much higher than the 8% for ICD / DSM bipolar disorders by considering patients that only had “bipolar depressions” as belonging to the same phenotype while these remain taken for unipolar by the international classifications. This illustrates the strength of a phenotypic description that is coherent within families.
Cycloid psychoses
Cycloid psychoses are bipolar phenotypes with purely relapsing-remitting course. Three different cycloid psychoses are described. They can be classified according to the mainly affected neuropsychological domain:
- Psychomotricity: hyperkinetic-akinetic motility psychosis,
- Affectivity: anxiety-happiness psychosis,
- Thought processes: excited-inhibited confusion psychosis.
Cycloid psychoses represent about 20% of all endogenous psychoses. Their clinical manifestations are highly polymorphic, usually with symptoms changing from time to time during the episode, even switching from one pole to the other, sometimes in the lap of a few seconds. This can lead to double-faced symptoms like ideas of self-sacrifice reflecting both anxiety and ecstasy, but the two opposite poles never fully coexist at the same time in the same patient. The polymorphism is due to changes in symptoms’ intensity while the symptomatic spectrum itself is more typical and restricted than the one of MDP. These phenotypes found their roots in the “bouffées délirantes aiguës des dégénérés” (acute delusional outburst of the degenerates) described by Valentin Magnan. Both concepts were supposed to be included in the ICD-10 diagnosis of acute and transient psychotic disorders or ATPD (F23), especially by the two polymorphic sub-types: without (F23.0) and with schizophrenic symptoms (F23.1). However, whereas cycloid psychoses are true phenotypes, i.e. longitudinally defined, ATPDs are only clinical presentations, i.e. cross-sectionally defined. One third of the “bouffées délirantes aiguës” will switch to schizophrenia or schizo-affective disorder diagnoses after 10 years’ follow-up, and this is also the case for half of the ATPDs after 5 years’ follow-up. Moreover, it has been shown that ATPDs do only overlap with “bouffées délirantes aiguës” and cycloid psychoses diagnoses in half of the cases. At last, it should be reminded that hyperkinetic-akinetic motility psychosis best matches with ICD/DSM’s catatonia. It is therefore not surprising that catatonia, even its schizophrenia subtype (F20.2), has a good prognosis according to ICD/DSM. This is in contradiction with the very poor prognosis of Kraepelin’s catatonic forms.
Psychotic episodes are usually, but not strictly, of short duration, lasting about 3 months on average in the pre-neuroleptic era. Acute onset and acute ending are seen in up to two thirds of the cases but these two features are neither sensitive nor specific.
Antipsychotics shorten most of the episodes but should be used with caution in akinetic motility psychosis which is particularly at risk for neuroleptic malignant syndrome. Antipsychotics are also effective for relapse prevention, but patients suffering from cycloid psychosis are very sensitive to their side effects. Maintenance of high or even moderate dosage, beyond the resolution of the episode, can cause abulia, so that otherwise fully remitted patient may look like “residual schizophrenia”, or can prompt a “post-psychotic depression”. On the other hand, once maintained for more than several months, discontinuing antipsychotics without a 1 to 2 years tapering period, increases the risk of relapse to a point that was unknown in the pre-neuroleptic era. These raised the hypothesis of neuroleptic-induced supersensitivity psychosis. There are alternative maintenance treatments since mood stabilizers confer the same degree of relapse prevention.
The relapsing-remitting course means that, in the inter-episode interval, patients have a slightly impaired global functioning with a GAF around 70 and develop full insight about the illness whereas no new symptom appears whatever the number of recurrences. It does not mean that the patients do not have any psychopathology when remitted. Indeed, they often have what Leonard called an accentuated personality or what Magnan saw as a sign of “degeneration”. But these differences in personality and cognition are inborn, pre-existing the episodes and are unaffected by the recurrence of episodes. As a group, patients have a lower average IQ with up to 10% of these patients quoting below 70. This comes with more frequent unspecific MRI abnormalities, e.g. enlarged ventricles, periventricular white matter hyperintensity or small cortical defects. These minimal brain damages are in accordance with the significantly higher proportion of mothers reporting infections of the upper airway during the first trimester of pregnancy, the increased frequency of childbirth complications and the seasonality effect relative to controls and non-system schizophrenias. There is a low heritability for these phenotypes with only 5% of affected first degree relatives, which is significantly different from MDP, cataphasia and periodic catatonia but non-significantly different from controls.
Patients affected by cycloid psychoses are more fragile and less resilient, making them vulnerable to relapse precipitating factors: stress, sleep disorder, cannabis, etc. Women are especially sensitive to estrogenic decrease: 88% of episodes start in the luteal phase of the menstrual cycle, which is significantly more frequent than for any other phenotype. It explains why cycloid psychoses account for 60% of postpartum psychoses with motility psychosis accounting for 36% on its own.
Phenotypes with build-up of residual symptoms: the schizophrenias
In the WKL perspective, the term "schizophrenia" carries a prognostic value as these phenotypes progress toward a persistent symptomatic state. Although abulia is a common feature of these residual states, it is frequently not central and can be absent in the beginning. They are better distinguished by specific long-lasting manifestations. Thus, this concept does not perfectly fit the Kraepelinian notion of “dementia praecox” of which cognitive blunting (“Verblödung”) is the hallmark. The terms system or non-system might be confusing since they have nothing to do with “systematized delusions”, i.e. the logical organization of delusional ideas. “System” must be understood in a more neurological sense, as a network dedicated to a define function, e.g. amyotrophic lateral sclerosis as the degeneration of the pyramidal system, or multiple system atrophy as the degeneration of extrapyramidal, cerebellar and vegetative systems. Because of their clear-cut and life-long unchanging (monomorphic) clinical manifestations system schizophrenias in the WKL perspective were interpreted analogically as the failure of 1 or 2 specific neuropsychological systems. As for their neurological counterparts, these systems are supposed to be distributed and hence do not correlate with specific cerebral localization.
Non-system schizophrenias
Four fifth of non-system schizophrenias have a progressive-relapsing course while one fifth may be primary progressive with barely detectable episodes. All have a specific heredity burden, without crossed liability. Moreover, in non-psychotic relatives, especially in obligate carriers, the same core residual manifestations than the relative’s phenotype can be observed, that are frequently taken for “unspecified” personality disorders. This might indicate that “psychosis” per se could be a mere by-product of the different pathological processes responsible for each non-system schizophrenia. As a whole, non-system schizophrenias benefit from both antipsychotics and mood stabilizers.
Affect-laden paraphrenia only accounts for 5% of endogenous psychoses but for about 10% of all ICD/DSM psychotic disorders. It may show up with a variety of different clinical presentations that have been identified independently by many authors around the world. To recall some of them, this phenotype mostly encompasses the “délire chronique d’évolution systématique” or chronic delusion of systematic course from Magnan, the specific erotomania delusion described by De Clérambault, the typical "Verrücktheit" or paranoia as described by Kraepelin, the “psychose hallucinatoire chronique” or chronic hallucinatory psychosis as reformulated by Henri Ey, the late paraphrenia from Roth, “Spätschizophrenien” or late-onset schizophrenia as described by Manfred Bleuler and rediscovered by American psychiatrists, etc… The reason why the WKL School considered these diverse clinical presentations to be the expression of the same phenotype is based on the parsimony’s principle, further specified in the “longitudinal principle” and the “familial aggregation principle” (see below). The core of this phenotype is a specific pathological affect which often begins with anxiety or/and ecstatic states and inevitably progresses to mistrust, irritability and hostility. Its classical residual picture is an irritated reference syndrome (“gereiztes Beziehungssyndrom”) although “Beziehungssyndrom” should be understand here as “a logical delusional construction about intentions of specific others regarding oneself”. Acute episodes typically come with multimodal hallucinations, including false memories and often more or less systematized delusions (in the classical sense). These are often bipolarly shaped including both ideas of persecution and grandiosity but are always strongly anchored in the affect. Judgment errors up to the acceptance of fantastic ideas contrast with a generally well organized thought process, a feature that has impressed many authors. The course is mostly progressive-relapsing, i.e. times of denying delusions, though never correcting them fully, and altogether slowly deteriorating over a 10 to 30 years period with more and more pervasive irritated reference syndrome up to fantastic delusional ideas. Regarding the international classifications, these patients are mostly diagnosed as (paranoid) schizophrenia, chronic delusional disorder and psychotic disorder not otherwise specified.
It is the only WKL’s phenotype affecting more females than males with a ratio of 3 women for 1 man, and for which the course is more quickly and severely deteriorating in females. This schizophrenic phenotype is also the most sensitive to antipsychotics with 84% of responders. The age of onset is highly variable with a median around 36 years, but with a large disparity explaining late beginners. The phenotype shows some familial aggregation, with 12% of affected siblings but only 2% of affected parents. This recessive heritability with incomplete penetrance pattern is further supported by a significantly larger number of patients born from consanguineous weddings (3.3% vs 1% for the other schizophrenias and cycloid psychoses) while consanguinity might be even greater in multiplex families (72%).
Cataphasia is a slightly more frequent phenotype accounting for about 8% of endogenous psychoses which gives an estimated prevalence of 0.1 to 0.2% in Germany. It is a bipolar phenotype mainly affecting thoughts and language. Its excited pole has been described by Kraepelin under the label “schizophasia”. If the symptomatology is commonly dominated by one pole in one patient, the two poles can be seen in multiplex families. It was again the familial aggregation principle that revealed the relation between the clinical picture of schizophasia and its counter-pole dominated by thought inhibition. The core of the phenotype consists in a disturbance in discursive organization as well as logical structure of the train of thought and a specific language disorder affecting both syntax and semantics. These core symptoms are regularly obvious during excited episodes, but need to be specifically looked for between the episodes. In fact, they only slowly accumulate, showing up perhaps only in the course of a long open conversation, and might otherwise remain discrete as they usually do not come with behavioral disorganization. During the episodes, the patients might present with a variety of affective and psychotic symptoms which explains why they are usually labelled with any ICD / DSM diagnosis between mood disorders and psychotic disorders (even catatonia in case of severe thought inhibition). As the disease progresses, persistent psychotic symptoms might remain mostly as fluctuating persecutory ideas and verbal hallucinations. The thought disorder may lead to a lack of understanding of the surrounding as it is seen in aging dementia or in partially remitted Wernicke aphasia.
The language disorders are quasi-pathognomonic, especially semantic errors. These can be verbal paraphasias, i.e. the inappropriate use of words of only grossly similar meaning which makes the understanding of the sentence uncertain. But these can also come up to the buildup of neologisms which in order to become diagnostically relevant should neither be deliberately metaphorical or poetic nor be “technical”, i.e. the regular use of the same new words to designate always the same (idiosyncratic) concept. Syntactic errors could also occur and might be easier to detect in languages with rather rigorous syntax. The “though and language test”, a standardized examination of formal thought which is a general instrument used by the WKL School to assess thought and language disorders, greatly sensitizes the detection of cataphasia. However, the significance of the errors depends much on the patient’s language skills which are consequently harder to ascertain in non-native speaking or low IQ patients.
Psychotic symptoms in cataphasia are sensitive to antipsychotics with 78% of responders. Males are more frequently and more severely affected than females with a ratio of 1 woman for 3 men which might reflect gender differences in language vulnerability to brain lesions. Thought disorganization associated with emotional turmoil makes cataphasic patients particularly at risk for suicidal behavior (52% of patients) and deaths by suicide (18% of patients). The phenotype shows familial aggregation, with 15 to 25% of affected first degree relatives, on top of which 12% of non-psychotic first degree relatives also show the typical thought and language disorder. Thus, if the core phenotype only consists in the residual symptoms, i.e. considering the affective and psychotic manifestations as unspecific and variable brain reaction to a cryptogenic pathological process, the cumulative amount of affected first degree relatives would reach 37%. In accordance with their “fundamental” thought and language disorder, remitted cataphasic patients have a bilateral reduction of cerebral blood flow in the temporo-parietal junctions when compared to controls and periodic catatonia patients treated by similar doses of antipsychotics. The same regions are also massively functionally disconnected with all the peri-sylvian cortices.
Periodic catatonia is roughly as common as cataphasia, accounting for about 7% of patients suffering from endogenous psychoses. The core of this phenotype is a specific psychomotor disorder of typical bipolar progressive-relapsing course. Despite its name, WKL’s periodic catatonia has nothing to do with the recurrence of IDC / DSM catatonic episodes. The international literature is further confusing as Gjessing used the same label to describe patients with such recurrences, a phenotype that would be diagnosed mainly as motility psychosis in the WKL’s perspective. Often subtle but unique qualitative psychomotor disturbances are typically overlooked or taken as medication side-effects while quantitative psychomotor disturbances are interpreted as affective manifestations. Hence the ICD / DSM catatonia diagnosis is rarely made in periodic catatonia. Conversely, the ICD / DSM bias towards behavioral or speech disorganization as well as affective or “psychotic” manifestations explains why patients with periodic catatonia are frequently diagnosed with depressive, bipolar, schizoaffective, schizophrenic, or not-otherwise specified psychotic or affective disorders. However, affective symptoms, thought disorder or transient hallucinations are never at the core of the symptomatology which is always characterized by qualitative psychomotor abnormalities. Residual symptoms are discrete at the beginning but progress as the episodes repeat. They are dominated by a generally diminished incentive (abulia) with reduced emotional expression which is intermingled with increased impulsivity, occasionally accompanied by more specific psychomotor symptoms, e.g. grimacing or parakinesias. Conversely, residual psychotic symptoms are rare and social or occupational impairment is altogether mild on average with a GAF of 60 ±20. At the beginning, if episodes are discrete, patients might be diagnosed as schizotypal personality disorder.
Typical neuroleptics are moderately efficient with 60% of responders, but this phenotype shows the largest response increment after switching to clozapine. Several studies have confirmed its high heritability, with 21-26% of affected first degree relatives, which is significantly larger than for system catatonias. In addition, if non-psychotic relatives showing psychomotor or personality disorder are considered, the percentage raises to 32-41% of affected first degree relatives. A genome-wide linkage study found evidence for a major susceptibility locus on chromosome 15q15 in most of the pedigrees assigning this phenotype to MIM 605419 in the Mendelian Inheritance in Man catalogue. But there are evidences for genetic heterogeneity as at least one other locus on chromosome 21q13-ter has been reported on the small set of pedigrees not related to chromosome 15. On the pathophysiological level, in relation with their residual symptoms, remitted patients have an increase of cerebral blood flow in the left insular, sensori-motor, premotor cortices relative to controls and patients with cataphasia equally treated with antipsychotics. The involvement of these regions in the pathophysiology of periodic catatonia is further suggested by the large improvement of residual symptoms by correcting this hyperactivity with rTMS.
System schizophrenias
Finally, system schizophrenias account for about 21% of inpatients with endogenous psychoses. The onset is generally characterized by an initial process phase of 1 to 5 years during which unspecific dysthymic and psychotic symptoms add to the progressive emergence of the typical clinical picture. Once established, the latter will remain unchanged up to the end of the patient's life. These clinical pictures are various with sixteen basic phenotypes accounting for about two thirds of these forms, and thirty-six possible combinations of two basic forms each accounting for the last third:
- There are six major phenotypes of system paraphrenias. These mainly consist in chronic paranoid clinical pictures which can combine in fifteen different pairs.
- The four phenotypes of hebephrenias share a specific disturbance of affectivity which leads to affective flattening with loss of initiative and ethical dulling. They can combine in six different pairs.
- System catatonias consist in six varieties of definite psychomotor impairment which may combine in fifteen different pairs.
Because of their deficit outcome and their clinical presentation sometimes in absence of any psychotic symptoms in the ICD/DSM sense, some forms of hebephrenias and catatonias are taken for personality disorders. Other forms would fit ICD diagnosis of “simple schizophrenia” (F20.6); Its DSM counterpart of “simple deteriorative disorder” disappeared from the 5th edition. The level of disability associated with system schizophrenias is severe, with few exceptions however.
Although the average age of onset is about 24, system catatonias can have a very early beginning and can be diagnosed in the autistic spectrum when ICD/DSM criteria are applied. Hebephrenias have a more limited range of onset during adolescence up to early adulthood with an average age of 23. System paraphrenias begin later at a mean age of 36. Except for parakinetic catatonia, no hereditary burden has been reported. The percentage of 2% to 4% of affected first-degree relatives is not significantly different from what is seen in controls but significantly different from periodic catatonia. In system catatonias, 34% of the mothers report an infection of the upper airways during the second trimester of pregnancy which is significantly larger than the 8% in periodic catatonia. Neuroimaging reveals significantly more cortical atrophy in system schizophrenias than in non-system phenotypes. Finally, antipsychotics are poorly effective, ranging from 1% to 40%, without advantage for clozapine. There is also poor benefit from mood stabilizers and antidepressants contrary to the other phenotypes.
Construction of the WKL classification
Although the final elaboration of the classification was Karl Leonhard’s contribution, nothing could have been done without the preliminary work of Carl Wernicke and Karl Kleist. This direct filiation over three generations does not mention the influence of Emil Kraepelin. However, it was not the mere dichotomy, introduced in the 6th edition of his “Lehrbuch”, that was influential as for the ICD/DSM, but for his latter and largely unknown attempt to refine the clinical pictures as detailed in his 8th and last edition. Following Wilhelm Griesinger, all these authors have in common the strong a priori that endogenous psychoses are “brain diseases”, a postulate that the phenomenologist Karl Jaspers criticized as “brain mythology” (“Hirnmythologie”).
Carl Wernicke (1848-1905): elementary symptoms and the principle of parsimony 1
Carl Wernicke endeavored to describe clinical presentations as precisely as possible. He introduced many clinical refinements allowing to distinguish between apparently similar manifestations. Following most of the psychiatrists of this period, Wernicke adopted the subdivision of mental activity into three main “neuropsychological” domains: emotions, thoughts, and psychomotricity. His neuro-psychological skills, acquired on the brain damaged patients from the 1870’s Franco-German war, guided his clinical examinations.
Elementary symptoms and symptom-complex interpretation
Wernicke postulated that some symptoms were closer to the core cerebral correlate which he called elementary symptoms (“Elementarsymptome”) from which others could arise. This idea was later rephrased by Eugen Bleuler, as primary and secondary symptoms. Following the principle of parsimony, or “Ockham's razor” which postulates that among competing hypotheses, the one which needs the fewest assumptions should be selected, Wernicke assumed that mental illnesses only affect a limited part of brain functioning. He tried to assign elementary symptoms to one neuropsychological domain from which secondary symptoms could result. As for classic medical syndromes, symptoms do not have diagnostic significance per se, but only as part of a “Symptomkomplex” or “symptom-complex”. The counterpart of this integrative approach is the highly differentiated symptomatology that comes along.
Let us illustrate this idea with the clinical presentation of a motionless and mute patient, with a ICD / DSM diagnosis of catatonia. In the WKL perspective, the same global picture can arise from the dysfunction of any neuropsychological domains. In the case of a primary impairment of psychomotricity, specific “elementary symptoms” of psychomotor inhibition must be present. For example, in inhibited motility psychosis, reactive and expressive movements are more affected than the voluntary ones, e.g. facial expressions appear “empty”, i.e. do not reflect any emotion, blinks or postural readjustment are reduced while prompted voluntary movements remain proportionally spared. Alternatively, motion poverty and mutism can also arise from “elementary” thought inhibition. In this case, voluntary movements are reduced secondarily to thought emptiness, whereas automatic movements are unaffected or even increased due to a release phenomenon, e.g. stereotyped movements. A perplexed facial expression reflects a worrisome lack of understanding, a state of mind that the patient will be in trouble to recall once remitted from the acute state. Finally, an “elementary” overwhelming affect emerging either from severe depression, anxiety or ecstasy, can secondarily paralyze all mental and psychomotor activity. But in this case the affect will be expressed in the patient’s postures and facial expressions and should be recalled after remission.
This first declension of the principle of parsimony applied to the clinical presentation gives a new dimension to the clinical approach. However, diagnosis cannot be done from a mere symptoms check-list but symptoms and signs need to be interpreted as part of a neuro-psychologically founded and coherent ensemble.
Karl Kleist (1879-1960): longitudinal study and the principle of parsimony 2
While only his assistant for a year, the Alsatian Karl Kleist took over Wernicke’s legacy. Kleist further developed these meticulous clinical observations also structured by his neuro-psychological expertise acquired on the brain damaged patients of World War I. His leading contribution was the conception of the longitudinal principle and its operationalization through long-lasting observations of patients during the thirty years he held the chair of psychiatry in Frankfurt (1920-1950).
Longitudinal or diachronic principle
The longitudinal principle is the second derivative from the principle of parsimony applied to the time course. It assumes that even if an individual presents several clinical pictures over time, he is unlikely to be affected by different pathologies but rather by the same one, presenting yet with different manifestations. Importantly however he differentiated between monomorphic and polymorphic phenotypes. It is a more flexible concept than the “systematic course” established as a principle by Jean-Pierre Falret in France (“marche systématique”) and Karl Kahlbaum in Germany (“Syndrom-Verlaufs-Einheit”) from Bayle’s description of general paralysis raised as a model. The systematic course principle is subsumed to the longitudinal principle but add two other constrains: a rigid pattern of symptomatic evolution and the an “outcome principle”, i.e. that patients should end-up in the same terminal state. This “outcome principle” was put forward by Emil Kraepelin to set up his dichotomy. The latter was not completely abandoned since as already stated, it made it possible to distinguish the different schizophrenia phenotypes as forms with symptomatic progression.
The longitudinal principle allowed Kleist to gather Wernicke’s clinical presentations into life-long phenotypes with specific course. The greatest success was the gathering of bipolar forms such as the MDP and the cycloid psychoses into life-long stable phenotypes and their separation from monopolar forms. The integration of the above-mentioned principles also enables to describe the three major courses:
- Relapsing-remitting course in which the patient gets back to his pre-episode state without residual symptoms whatever the number of episodes, e.g. MDP, monopolar mood disorders and cycloid psychoses.
- Progressive-relapsing course, for which the repetitions of acute episodes are followed by incomplete remissions and occurrence of increasing residual symptoms, e.g. non-system schizophrenias.
- Primary progressive course in which the monomorphic residual state gradually takes place over a 1 to 5 years “process phase”, e.g. system schizophrenias.
Karl Leonhard (1904-1988): familial study and the principle of parsimony 3
Leonhard conceptually contributed to the classification by the addition of the familial aggregation principle which he put into practice to end up the classification.
The familial aggregation principle
The familial aggregation principle is the third derivative from the principle of parsimony applied to multiplex families. Leonhard postulated that if several members of the same family present with an endogenous psychosis, they are likely to share the same liability. He actively and systematically gathered the clinical descriptions of the affected first degree relatives of multiplex families trying to describe familiarly coherent phenotypes as illustrated by the case vignettes of his classification textbook. This simple idea allowed him the last breakthrough on non-system schizophrenias by the description of their core phenotypic features, shared among affected family members. According to this principle Leonhard was able to group together the four forms of affect-laden paraphrenia described by Kleist into one common phenotype based on the fact that they were observed in different members of the same multiplex family. The same principle allowed him to identify and describe the poorly characteristic “dazed” clinical picture as the inhibited counterpart of Kraepelin’s schizophasia leading to the creation of the coherent phenotype of cataphasia. At last, the familial aggregation principle was also the key to refine the differential diagnosis between periodic catatonia and motility psychosis.
A step by step empirical construction finalized in 1968
The different phenotypes did not emerge at once out of the blue. The empirical nature of the phenotypic description is illustrated by the step by step gathering of clinical presentations and the refinements of the differential diagnoses, that were based on observations and guided by the aforementioned principles.
The monomorphic primary progressive forms (1936)
System schizophrenias were the first to be described. Their primary progressive course, ending within few years in an unchanging monomorphic clinical picture simplified their description. As being the core of “dementia praecox”, Emil Kraepelin already proposed a first classification of their different clinical presentations in the 8th edition of his "Lehrbuch". Kleist expanded it and introduced the hypothesis of simple and combined neuropsychological systems injuries. Leonhard resumed and refined the phenotypic description helped by his frequent visits in long-stay psychiatric hospitals where most of these chronically disabled patients were living. The initial phenotypic description of his habilitation thesis performed under Kleist’s supervision remained the foundation, although many refinements came later from further observations.
The monopolar relapsing-remitting forms (1949)
Kraepelin's manic-depressive illness was a catch-all for all remitting psychoses. Their clinical presentations were described as any combination of excitation or inhibition of the different neuropsychological domains. The longitudinal principle made it possible to distinguish monopolar ("einpolig”) vs. bipolar (“zweipolig") phenotypes though Kraepelin did not seem to believe in the need to distinguish monopolar and bipolar forms. Kleist´s concepts in this regard were first synthetized by Edda Neele (1910-2005) in her habilitation thesis. The full description of monopolar phenotypes was achieved first since they were simpler to describe as invariant during an episode and identical from one episode to the other.
Bipolar relapsing-remitting forms (1957)
It took a little bit longer to come to a more definitive description of the bipolar relapsing-remitting forms, i.e. MDP and cycloid psychoses. The latter was a major restructuring of the classification with motility and confusion psychoses, formerly part of Kleist’s marginal psychosis (“Randpsychose”), brought together with anxiety-happiness psychosis. This new family, renamed by Leonhard under Kleist’s label of “cycloid psychoses”, gather phenotypes that have in common bipolar syndromes with characteristic psychotic disorders of affect, thought or psychomotricity which extended beyond the clinical manifestations of MDP while presenting a purely relapsing-remitting course.
Non-system schizophrenias (1961)
The major final step was the description of the “schizo-affective” bipolar progressive-relapsing forms which proceed toward specific residual states. These were difficult to separate from cycloid psychoses because they shared many features while the progression might not be clearly perceptible during early stage of the illness. Last, non-system schizophrenias can only show up one symptomatic pole in a single patient, hence the decisive contribution of the familial aggregation principle to characterize them.
The final version of the classification was published in 1968 and no changes have been made since. All the following works sought to enrich the phenotypic description and to look for biological correlates.
Reproducibility
Reliability of WKL phenotypes or inter-rater reliability
The inter-rater reliability is a poor marker of face validity but a technical requirement for a phenotype to be scientifically usable (neopositivism). On average, WKL phenotypes are highly reliable with 97% of inter-rater diagnostic consistency giving an average kappa value of 0.82 to 0.93. In comparison, reliability assessment of the ICD and the DSM’s less numerous categories gives kappa values of 0.84 for schizophrenia, of 0.71 to 0.83 for bipolar disorder but of 0.22 for schizo-affective disorder.
These excellent results must be tempered by the fact that reliability assessment has been performed with trained raters from the same university. Training is undoubtedly the stumbling-block for the world-wide diffusion of this phenotypic classification. Thoroughly studying the reference book is the basis, but alone not sufficient. Since the text uses many psychopathological concepts that have been neglected by ICD/DSM psychiatry and does not give all the cues and skills for the interpretation of the clinical presentation as coherent symptom-complex, the guidance of a tutor is strongly recommended.
Test-retest reproducibility and stability
Diagnosis stability of chronic psychiatric manifestations is a primary requirement for natural phenotypes. Considering the question on a purely operational level, as it is done for ICD / DSM, it can be assessed by test-retest reproducibility. On retrospective chart review, 90% of the patients having an initial ICD diagnosis of schizophrenia had a consistent diagnosis among the episodes on 25 years average follow-up. WKL classification stands well in comparison, since in systematic prospective studies, the test-retest reproducibility at 15 years follow-up was of 93% and ranged from 76 to 93% at 33 years follow-up with the exception of system paraphrenias which were only reproduced in 68% of the cases.
However, the question of diagnostic stability can be considered the other way around in the WKL perspective. Here diagnostic changes are not considered as phenotypic changes but as diagnostic errors. Indeed, the longer the follow up, the larger the collection of clinical information and the higher the certainty of WKL diagnosis.
Conclusion
For those who wish to remain in the traditional paradigm of scientific medicine, the WKL School describes natural phenotypes that should be attractive starting points for researchers and predictive tools for clinicians. They have a sufficient reliability. They are observation-driven phenotypic descriptions, based on neuropsychological knowledge and optimized on three derivatives of the principle of parsimony: the elementary symptoms, the longitudinal and the familial aggregation principles. Theses phenotypes have a good predictive validity, but also clear demonstrations of further differential validity, e.g. age of onset, heritability without crossed liability, potentially brain-deleterious events during pregnancy and specific response to treatments. Finally, first biological correlates have been reported but deserve replications. Karl Leonhard’s classification is still a source of inspiration and deserves to be better known especially in the scientific community.
References
Foucher JR, Gawlik M, Roth JN, de Billy C, Jeanjean LC, Obrecht A, Mainberger O, Clauss JME, Elowe J, Weibel S, Schorr B, Cetkovich-Bakmas M, Morra C, Rebok F, Ban T, Bollmann B, Roser MM, Hanke M, Jabs BE, Franzek EJ, Berna F, Pfuhlmann B. "Wernicke-Kleist-Leonhard phenotypes of endogenous psychoses: a review of their validity". Dialogues Clin Neurosci. 2020;22(1):37-49. An introduction to Leonhard's classification.
Foucher JR, Jeanjean LC, de Billy CC, Pfuhlmann B, Clauss JME, Obrecht A, Mainberger O, Vernet R, Arcay H, Schorr B, Weibel S, Walther S, van Harten PN, Waddington JL, Cuesta MJ, Peralta V, Dupin L, Sambataro F, Morrens M, Kubera KM, Pieters LE, Stegmayer K, Strik W, Wolf RC, Jabs BE, Ams M, Garcia C, Hanke M, Elowe J, Bartsch A, Berna F, Hirjak D. The polysemous concepts of psychomotricity and catatonia A European multi-consensus perspective. European Neuropsychopharmacology. 2022; 56(3):60-73. (supplément).
Reactions: on the international network for history of neuropsychopharmacology (INHN).
- Edward Shorter’s comment on Jack R. Foucher et al.’s paper on Wernicke-Kleist-Leonhard phenotypes of endogenous psychoses. INHN. 2020, May 7.
- Authors' answer n°1: Metatheses of the Wernicke-Kleist-Leonhard research program. INHN. 2020, October 15.
- Hector Warnes’ comment on Foucher et al’s reply to Edward Shorter’s comments. INHN. 2020, November 19.
- Authors' answer n°1: Differentiated psychopathology: a splitter methodological metatheory. INHN. 2021, May 13
- Authors' answer n°2: WKL symptom-complexes vs positive and negative symptoms. INHN. 2021, May 20.
- Hector Warnes’ response to Jack R. Foucher’s reply about elementary/primary symptoms. INHN. 2021, September 30.
- Hector Warnes’ comment on Foucher et al’s reply to Edward Shorter’s comments. INHN. 2020, November 19.
- Authors' answer n°2: ICD-DSM catatonia disorder and WKL-periodic catatonia phenotype: Struggling with (in)commensurability. INHN. 2020, November 12.
- Authors' answer n°1: Metatheses of the Wernicke-Kleist-Leonhard research program. INHN. 2020, October 15.
- Barry Blackwell’s comment. INHN. 2020, September 3.
- Hector Warnes’ comment. INHN. 2020, September 3.
- Barry Blackwell’s additional comment. INHN. 2020, November 5.
- Hector Warnes’ additional comment on Edward Shorter’s comment. INHN. 2020, November 12.
- Carlos R. Hojaij’s comment. INHN. 2020, November 12.